If Gardasil 9 proves to be safe and effective against the HPV types for which it is
designed to confer immunity, then it will offer substantially more protection against
cancer-causing strains of HPV than original Gardasil. Even so, at best it will prevent
only about 35% of HPV infections with high-risk (cancer-causing) strains of HPV.
That sounds worthwhile, but our experience with the original Gardasil shows that some caution is in order. Look at Markowitz's table 3. Look at the lines labeled "Vaccinated" and compare them with the lines labeled "Unvaccinated," in this excerpt from the table:
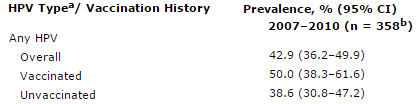
Do you see it? The vaccinated patients have the highest HPV infection rates! The overall prevalence of HPV among vaccinated sexually-active teens is 50.0%, but among unvaccinated sexually-active teens it is only 38.6%.
The prevalence of high-risk HPV strains other than 16 & 18 is similarly skewed: 35.2% of vaccinated sexually-active teens are infected, and only 25.3% of unvaccinated sexually-active teens. Vaccinated teens had much lower rates of type 16 & 18 infection than did unvaccinated teens, indicating that the vaccine does work as designed against those strains, but that wasn't sufficient to offset the vaccinated teens' higher rates of infection with other high-risk types. Because most high-risk HPV infections are types other than 16 and 18, a slightly higher percentage of vaccinated teens had high-risk HPV infections than did unvaccinated teens. (I speculate that the cause might be that the behavioral effects of the perceived "protection" worsened the risk of infection by more than the immunity to types 16 & 18 lessened the risk.)
(Note: that does not necessarily mean that Gardasil vaccination increases cancer risk; see:
http://www.burtonsys.com/gardasil--ltr_to_joann1.html)
Those studies were done with the original, quadrivalent Gardisil. Hopefully, the results will be better for Gardasil 9. But the fact remains that vaccination offers only weak protection against infection with high-risk strains of HPV.
Additionally, original Gardasil has its own risks, which Gardasil 9 presumably shares:
- http://www.judicialwatch.org/press-room/weekly-updates/27-judicial-watch-special-report-hpv-vaccine-gardasil/
- https://www.cbsnews.com/news/gardasil-researcher-speaks-out/
- https://pop.org/gardasil-guards-against-almost-nothing-merck-researcher-admits/ (or here)
The number of deaths and injuries is small compared to the number of patients, but it could eventually be dwarfed by the number of future cancer deaths, if some patients mistakenly believe that vaccination means they needn't get regular exams & pap smears.
Neither orginal Gardasil nor Gardasil 9 reliably protect women from cervical cancer. They will not eradicate that disease, nor even come close. The best we can hope for is a modest reduction in the number of cases, and even that is uncertain.
Over-hyping the potential of these vaccines to combat cervical cancer could end up
killing more patients than the vaccines save:
http://www.burtonsys.com/gardasil--ltr_to_drphilips2.html
Dave Burton
![]()
W: +1 919-481-0149
M: +1 919-244-3316
109 Black Bear Ct, Cary, NC 27513-4941 USA
December 16, 2014
Last updated: March 12, 2015